Bariatric surgery (also called metabolic or weight-loss surgery) refers to procedures that help people lose weight by making the stomach smaller or rerouting the digestive tract. The most common operations are gastric sleeve gastrectomy, Roux-en-Y gastric bypass, and adjustable gastric banding. In a gastric sleeve, about 80% of the stomach is removed, leaving a narrow “sleeve” so you feel full after eating little. In gastric bypass, the surgeon creates a small stomach pouch and connects it to the mid-intestine, bypassing most of the stomach and upper bowel so that fewer calories and nutrients are absorbed. All of these surgeries work by restricting food intake, often with hormonal effects that reduce appetite. They are major surgeries but are generally safe when performed by experienced bariatric teams.
Bariatric surgery is indicated for people with severe obesity. In general, candidates have a body mass index (BMI) of 40 or more, or a BMI of 35–39.9 with serious obesity-related health problems (such as type 2 diabetes, high blood pressure, or sleep apnea. For example, the U.S. National Institutes of Health (NIH) specifies surgery for BMI ≥40, or BMI ≥35 with illnesses like diabetes or heart disease. Some guidelines and insurers even consider surgery at BMI 30–34.9 if diabetes is poorly controlled. (One recent consensus recommends bariatric surgery regardless of comorbidities once BMI is ≥35, and considered for BMI 30–34.9 with metabolic disease) In practice, doctors will also look at factors like your weight history, previous diet attempts, and overall health. Insurance companies often require documented failed weight-loss efforts before approving coverage.
Bariatric procedures not only produce dramatic weight loss, but also often improve or resolve obesity-related conditions. As NIH notes, weight-loss surgery can help improve type 2 diabetes, high blood pressure, high cholesterol, heart disease, sleep apnea and joint pain. Many patients experience normalized blood sugar and reduced medication needs after surgery. In short, bariatric surgery is a tool for people with very high BMI who have struggled to lose weight by diet and exercise alone. It can be life-changing, but it requires commitment to lifestyle change afterwards.
BMI Criteria: Who Qualifies for Each Procedure?
Weight-loss surgeries generally use the same BMI criteria, but sometimes there are nuances by procedure. In most centers, both gastric sleeve and gastric bypass require similar criteria: typically BMI ≥40, or BMI 35–39.9 with at least one severe comorbidity (for example, diabetes, heart disease, severe sleep apnea). For instance, Duke Health notes insurers usually cover surgery only if BMI is ≥40, or BMI 35–39.9 and a major weight-related health issue. If you have BMI 30–34.9, surgery may still be considered when you have uncontrolled type 2 diabetes or other serious metabolic disease. (Newer guidelines even suggest considering surgery for select patients down to BMI ~30 with metabolic syndrome) Adjustable gastric banding (less common today) uses similar cutoffs. A gastric balloon (non-surgical, temporary implant) is often offered for patients with BMI ~30–40 who prefer a less invasive option.
Importantly, all candidates must be committed to change. Surgeons and insurers typically require you to show you’ve tried diet and exercise programs first. You also need a psychological evaluation to ensure you understand the risks and can follow the post-surgery plan. In short, qualifying for surgery means having medically significant obesity and the readiness to adopt a new lifestyle.
Preparing for Surgery: Medical, Psychological, and Lifestyle Steps
Before the big day, you will go through thorough pre-operative preparation. This multi-step evaluation ensures you’re safe and ready for surgery. Key pre-op steps include:
Medical evaluation and tests.
Your surgeon will order blood tests (complete blood count, metabolic panel, liver function, vitamin levels, etc.), diabetes evaluation (HbA1c), nutritional markers, and any needed imaging or cardiology tests (EKG, stress test). You’ll have a detailed physical exam focusing on your heart, lungs, lungs, abdomen, and overall health. This often includes checking for sleep apnea (a very common issue in obesity) and ensuring any conditions like hypertension or lung disease are controlled. In short, as one expert review notes, a “comprehensive medical evaluation” – including a meticulous history and physical exam of the cardiovascular, pulmonary, gastrointestinal and metabolic systems – is required.
Psychological assessment.
Since bariatric surgery significantly changes eating habits and lifestyle, a psychologist or psychiatrist will evaluate your mental health and readiness. This interview covers your weight history, eating behaviors (e.g. binge-eating, emotional eating), mood disorders, body image, and social support. It’s common for bariatric candidates to have anxiety, depression or disordered eating, and addressing these before surgery is important. Undergoing this evaluation helps uncover any issues that could interfere with recovery (for example, uncontrolled depression or untreated eating disorders). Importantly, having a psychological issue does not automatically disqualify you, but the team wants to plan support (counseling, medications, support groups) to help you succeed in the long run.
Dietary counseling and pre-op diet.
You will meet with a dietitian to learn the post-surgery diet plan and to start making healthy changes. Often the surgeon will prescribe a short “liver-shrinking” diet of clear liquids or very-low-calorie meals for ~2 weeks before surgery. This low-calorie diet helps shrink the liver and reduce abdominal fat, making the surgery safer and easier to perform. (For example, Cleveland Clinic notes: “If you’ve been approved for a gastric sleeve, the next step will be a two-week liquid diet… The purpose is to lose some of the fat in your abdomen and your liver to make the surgery safer.”) You’ll also practice the strict diet progression that you’ll follow after surgery – starting liquids, then purees, then soft foods – so that it becomes second nature.
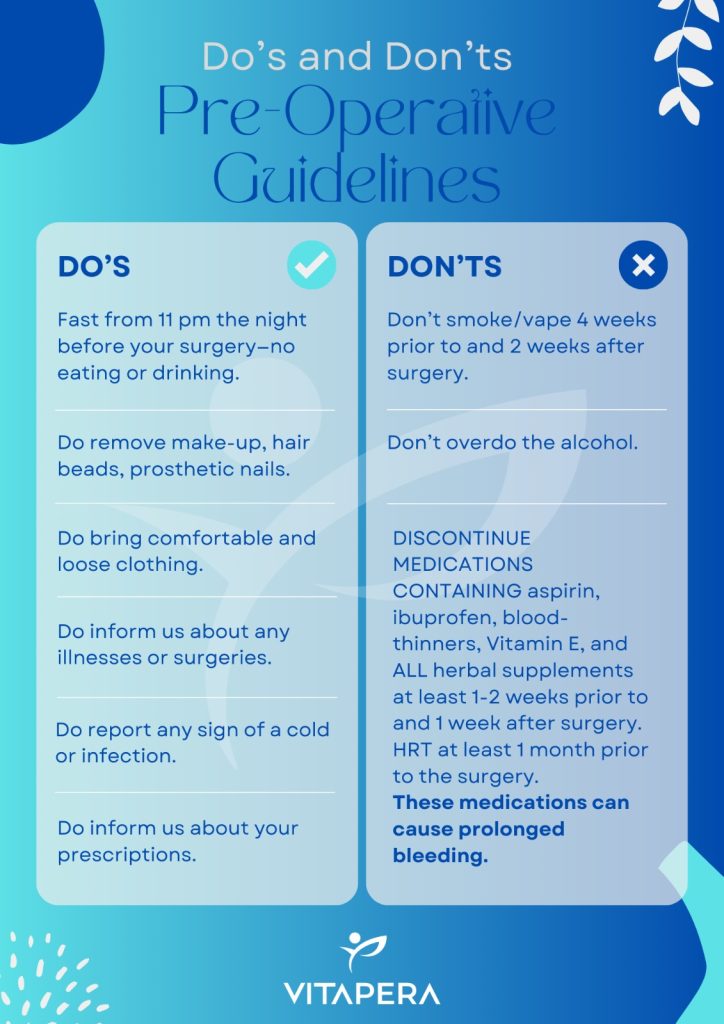
Lifestyle changes.
You will be asked to make some important changes before surgery. Most programs require stopping smoking at least 4–6 weeks pre-op, since tobacco greatly increases surgical risks. Avoiding alcohol is also strongly advised. Your doctor will tell you to stop or taper certain medications, especially blood thinners (aspirin, NSAIDs, some supplements) at least a week before surgery to reduce bleeding risk. Any vitamin or nutrient deficiencies discovered in your bloodwork will be corrected beforehand (for example, low iron or vitamin D). In many cases, you’ll also be advised to start a modest exercise plan or weight-loss effort to improve fitness, since insurers often look for a history of trying diet/exercise.
Support and education.
You may attend educational classes or join a support group run by the bariatric team. These prepare you mentally and practically for surgery. Topics include how to eat after surgery, how to handle hunger and emotions, and how to avoid complications. Meeting other patients who have gone through the process can be reassuring. (In fact, many bariatric centers say “many patients benefit tremendously from our bariatric surgery support group…” which meets monthly to discuss challenges.)
By completing all these steps (medical clearance, psych clearance, diet initiation, etc.), you’ll be ready on surgery day. This preparation reduces risk and sets you up for success in your weight-loss journey.
What to Expect on Surgery Day and During Your Hospital Stay
On the day of surgery, you’ll arrive early at the hospital. After checking in, nurses will place an IV line and you will meet your anesthesia team. Under general anesthesia, the surgery will be performed. Most modern bariatric operations are done laparoscopically – meaning the surgeon makes 3–5 small incisions in the abdomen and uses a camera and long instruments. Laparoscopic surgery (sometimes robot-assisted) has major benefits: smaller incisions, less pain, less bleeding and a faster recovery compared to open surgery.
Once the procedure is complete, you will wake up in the recovery room. Expect to feel groggy and have some discomfort, which will be managed by IV pain medications at first. You may have compression stockings or boots on your legs to prevent clots, and possibly a small drain in your abdomen if the surgeon places one. The care team will monitor your vital signs, breathing, urine output, and pain level. Within a few hours, when you are stable, you will be moved to your hospital room or continue recovery for the night.
Hospital Stay:
Most patients stay in the hospital about 1–2 nights after surgery (sometimes longer depending on individual needs). For example, after a gastric bypass, the average stay is about 1 day; for a sleeve it may be 1–2 days. During your stay, the main goals are pain control, early mobilization, and beginning your post-op diet. You will be encouraged to get out of bed and walk as soon as possible (often the same day) to reduce the risk of blood clots and pneumonia. You will also be taught breathing exercises (incentive spirometry) to keep your lungs clear. Nurses will assist you with a sit-up and short walk in the hallway within hours after surgery.
Diet:
Shortly after surgery you’ll start on very small sips of clear liquids (water, broth). Drinking slowly and staying hydrated is crucial. The first 24 hours usually involve clear liquids only. As you tolerate fluids and meet surgical milestones, you will advance to the prescribed diet: clear liquid → full liquid → pureed → soft solids → regular foods, over about 6–8 weeks. (For example, one clinic notes that patients spend several weeks on liquids and soft foods, and may not return to normal solid foods until 2–3 months after surgery) The medical team will provide detailed guidelines, but key points include avoiding sugars and starches (to prevent dumping syndrome) and focusing on high-protein fluids early on.
Recovery in Hospital:
You may have mild nausea or discomfort, which is common. Pain is usually most significant for the first 1–2 days and controlled with medication, then tapers quickly. Your bowel function may be slow at first; stools will be small due to reduced intake. It’s common to experience fatigue (your body is healing and on a low-calorie diet). Nurses will check on you frequently, change dressings, and help you use the restroom or a bedside commode. By the second day you should be able to walk, drink adequate fluids, and control pain with pills. At that point you will typically be discharged home with a clear understanding of home-care instructions. Your surgeon or nurse will review all instructions before you leave, including diet progression, activity limits, wound care, and signs of complications (fever, worsening pain, etc.).
Long-Term Follow-Up: Diet, Exercise, Vitamins, and Emotional Support
Bariatric surgery is just the beginning of a lifelong journey. Long-term success requires ongoing changes in diet, activity, and routines.
Diet and Nutrition: In the first 6–8 weeks after surgery, continue a staged diet as taught by your team: clear liquids → protein shakes/full liquids → pureed foods → soft foods → then regular healthy foods. Chew slowly, eat very small portions, and stop eating when you feel comfortably full. For life, you’ll need to follow a high-protein, nutrient-dense diet. Aim for at least 60–80+ grams of protein per day to preserve muscle mass. Drink plenty of water (generally ~64 ounces per day) between meals (avoid drinking at the same time as eating to prevent overfilling the stomach). Your dietitian will help you plan meals rich in lean protein (meat, fish, eggs, dairy or plant proteins), vegetables, and some whole grains or legumes if tolerated.
Avoid foods high in sugar, concentrated carbs or fat, as these can trigger dumping syndrome (rapid gastric emptying causing nausea, diarrhea or dizziness). Also avoid drinking alcohol (especially strong liquor), as it hits you faster and can add many calories. In general, you will eat much less than before, so each bite counts: focus on protein first, then vegetables, and minimize fillers like starch. You may also need to take prescribed multivitamin/mineral supplements for life.
Vitamins and Supplements: Because bariatric surgery reduces the amount of food you can eat and alters nutrient absorption, deficiencies are common without supplementation. Your surgeon will usually prescribe:
- A complete bariatric multivitamin/mineral (often with iron).
- Calcium citrate 1200–1500 mg per day plus Vitamin D (to protect bones).
- Iron (often with Vitamin C to enhance absorption) – important especially for menstruating women.
- Vitamin B12 (1000 mcg monthly or 350–500 mcg weekly by injection or sublingual).
For example, one expert source recommends for gastric bypass patients: a multivitamin, calcium + D, iron + C, plus B12; gastric sleeve patients generally need the same regimen. Your doctor will check blood levels (CBC, iron studies, B12, vitamin D, etc.) at intervals (often at 3 months, 6 months, and annually) to catch any deficiencies. Taking supplements every day is critical – skipping them can lead to anemia, osteoporosis, neuropathy and other serious issues. Your bariatric team will likely give you a detailed vitamin schedule and may recommend a specific bariatric vitamin brand to ensure you get adequate doses.
Exercise and Activity: Regular physical activity is a cornerstone of maintaining weight loss. Start gentle exercise early (walking most days, gradually increasing duration). Your surgeon or physical therapist will advise on when to resume specific activities (lifting restrictions usually ~6 weeks). Long-term, aim for at least 150 minutes per week of moderate exercise (e.g. brisk walking, swimming) combined with muscle-strengthening 2–3 times weekly. Research shows that bariatric patients who exercise regularly (about 60 minutes most days) lose weight more quickly and improve fitness. Exercise also builds muscle (which can otherwise be lost during rapid weight loss) and helps prevent weight regain. Many programs encourage patients to form exercise habits before surgery so they are established during the peak weight-loss phase.
Medical Follow-Up: You will see your bariatric surgeon or clinic regularly, especially in the first 1–2 years. Typical follow-up visits are at 1 month, 3 months, 6 months, 1 year, then annually. At these visits the team checks your weight loss progress, reviews your diet, monitors for complications, and orders lab tests. They also provide guidance on how to maximize loss or address any plateau. Beyond surgical follow-ups, continued care may involve your primary doctor (to manage chronic conditions), a registered dietitian (for meal planning), and possibly a psychologist if emotional issues arise.
Emotional and Social Adjustments: Significant weight loss can bring emotional changes. Many patients feel better psychologically – their self-esteem and mood often improve as health and mobility improve. However, surgery can also unmask emotional challenges that were “buffered” by excess weight. It’s normal to experience anxiety, stress or even a new “obsession” with food after surgery. For example, some people report preoccupation with what they eat or fear of gaining weight after bariatric surgery. Others feel vulnerable as their body changes (the “safety” that fat provided is gone). Physical changes – especially loose, sagging skin – can also cause self-consciousness. In fact, one study notes that patients often struggle with “self-consciousness about excess skin,” which can be mitigated by body-contouring surgery.
To manage these challenges, psychological support is important. Many centers offer support groups or counseling through the first year (and beyond). Connecting with others who have had bariatric surgery helps; as one program observes, “many patients benefit tremendously from our bariatric surgery support group” where people share experiences and coping strategies. Counseling or therapy (either individually or in a group) can help you develop healthy coping mechanisms for stress and food issues. Be aware that alcohol sensitivity increases after some bariatric procedures, and alcohol use is generally discouraged, as patients can become intoxicated more quickly and some turn to alcohol to cop.
Remember: bariatric surgery is a tool, but long-term success comes from changing your lifestyle and mindset. Having a supportive team (family, friends, medical providers) and staying engaged in follow-up care are key. At Vitapera, we emphasize patient education and support – we guide you to build new habits that fit your new stomach and your new life.
Body Contouring After Weight Loss: Liposuction & Mommy Makeover
After major weight loss, most patients find that stubborn pockets of fat and loose skin remain. Body-contouring surgery can help complete your transformation. The American Society of Plastic Surgeons explains that these procedures “address stubborn fat and loose, sagging skin to provide a more svelte appearance.” Common problem areas are the abdomen, thighs and arms: after losing 50+ pounds, these areas often have hanging skin that can even cause rashes or discomfort. Liposuction is used to remove any remaining fat deposits (for example, “trouble spots” on the belly or flanks), helping to sculpt your new shape. Surgical lifts and tucks remove excess skin and tighten the underlying muscles. For instance:
- Tummy Tuck (Abdominoplasty): Removes extra abdominal skin and tightens separated abdominal muscles, creating a firmer waist. Vitapera’s tummy tuck includes trimming excess fat and tissue and repairing muscle diastasis (a common issue after weight gain or pregnancy)
- Liposuction: Targets localized fat in the belly, hips, thighs, or back. We offer advanced VASER ultrasound-assisted liposuction to gently break down fat and sculpt the body with minimal trauma. (Keep in mind, liposuction is not for weight loss but for fine-tuning contours after you have lost most of your weight.)
- Arm Lift / Thigh Lift: Removes sagging skin from the upper arms or thighs, improving comfort and appearance. These lifts often accompany liposuction for best results.
- Breast Lift or Augmentation: Many patients (especially women) have deflated or sagging breasts after weight loss. A breast lift, with or without augmentation, can restore a more youthful shape.
- Mommy Makeover: This term refers to a customized combination of procedures (usually abdomen + breasts, and often liposuction) to rejuvenate a woman’s figure after pregnancy or after massive weight loss. For example, a typical Mommy Makeover might include a tummy tuck, breast lift/augmentation, and liposuction of flanks and thighs. It’s important that you be at or near your goal weight before contouring surgery, so that results last. (If you need to lose more weight, we advise waiting; conversely, post-surgery weight gain can stretch skin again.)
At Vitapera we specialize in post-bariatric contouring. Our Mommy Makeover packages in Turkey can include any combination of tummy tuck, breast enhancement, liposuction, Brazilian Butt Lift, and more – all tailored to your needs. We work with board-certified plastic surgeons who are experts in these complex procedures. The result is a smoother, tighter body that reveals the full payoff of your hard work. Many of our patients remark that once the excess skin is removed, “you finally see the person underneath,” giving a huge confidence boost.
Why Choose Vitapera & Istanbul for Your Surgery
Istanbul (and Turkey in general) has become a world-leading medical tourism destination. Turkey is known for affordable, high-quality healthcare. Many hospitals here have state-of-the-art technology and international accreditations (for example, Joint Commission International, JCI). Importantly, the cost of surgery in Turkey can be a fraction of what it is in Western countries. One report notes that medical treatments in Turkey are often 60–80% cheaper than in the U.S. or Europe For example, cosmetic surgery that might cost $10,000+ abroad often costs $2,000–$4,000 in Turkey – without cutting corners on safety or skill.
Vitapera combines these advantages with comprehensive patient care. Our packages include everything you need for a smooth experience:
- Expert surgical teams: We partner with JCI-accredited hospitals and board-certified bariatric surgeons in Istanbul, many of whom have trained internationally. You get top-tier medical expertise at very competitive prices.
- All-inclusive support: Vitapera arranges your logistics from start to finish. A private driver will pick you up at the airport and handle all transfers (to clinic, hotel, airport). A personal health consultant fluent in your language will assist you 24/7. Your luxury recovery hotel (with nutritious meals and comfort) is booked by us at no extra cost. In short, we treat you like VIPs.
- Affordability: Even after including flights and lodging, patients often save thousands of dollars. We provide clear package pricing so you know the cost up front.
- Patient-centered care: Our dedicated team (doctors, nurses, coordinators) stays with you through every step, from initial consultation to long after you return home. We offer lifelong follow-up: patients can always contact us with questions or concerns, even years later.
More than 20,000 patients worldwide have trusted Vitapera for bariatric and cosmetic procedures. We pride ourselves on high patient satisfaction and top clinical outcomes. When you choose Vitapera, you’re not just getting a surgery – you’re gaining a partner in your health journey. In beautiful Istanbul, you can transform your body and boost your well-being, all while enjoying excellent care and remarkable value.
Key Takeaways: Bariatric surgery can be life-changing for those with severe obesity, leading to major weight loss and health improvements. To qualify, you generally need a BMI ≥40 (or ≥35 with comorbidities). Preparation involves medical and psychological evaluations, specialized diets, and lifestyle changes. On surgery day you’ll have a laparoscopic procedure and stay in the hospital a day or two, then follow a strict diet progression. Long-term success requires dietary discipline, exercise, supplements (multivitamin, calcium/D, iron, B12), and emotional support. After weight loss, many patients benefit from body contouring (liposuction, tummy tuck, Mommy Makeover) to remove excess skin. Vitapera offers these plastic surgery options as part of its services. By coming to Istanbul with Vitapera, you get world-class medical care and patient support at a fraction of Western cost. Our team will guide and motivate you every step of the way – from your first evaluation through recovery and beyond – so you can achieve the healthier, happier life you deserve.